Contributors
Matt Dane,
DNP, MBA, RN
SVP of Business Development
Hallmark
Michelle Hereford,
MSHA, RN, FACHE
System Chief Nurse Executive
University Hospitals Health System
Michelle Sanchez-Bickley,
MS, SPHR, SHRM-SCP
Chief People Executive
Hallmark
Annalee Starks,
BSN, RN
System Director of Staffing
Franciscan Missionaries of Our Lady Health System
Michael Yost,
EVP
Chief Human Resources Officer
Great River Health
When it comes to nurse staffing and staffing other clinicians in healthcare settings, it’s a tough marketplace out there.
It’s getting worse by the year. Nurses are increasingly difficult to come by as turnover rates remain high and nurse shortages grow. This has fueled a yearslong increase in labor costs that, when paired with changes to reimbursement that are threatening revenues, are putting the financial sustainability of many hospitals, health systems, and other healthcare organizations at risk.
The good news is that these organizations have ample options for overcoming these clinical shortage challenges successfully. In particular, formulating flexible work programs for nurses who want more control over their work experience and deploying modern technologies can empower healthcare organizations with the tools and strategies they need to carve out financial and clinical success, even in today’s challenging climate.
But navigating the difficult labor landscape requires a proactive and informed approach. To help healthcare organizations both answer current and emerging challenges and take advantage of newfound opportunities, we submitted a range of pressing questions to experts from throughout the healthcare sector. Below, we have compiled the insights, forecasts, and strategic advice from their responses.

The Clinical Shortage Challenges of the Future
Nurse shortages and turnover among clinicians will continue to strain healthcare organizations.
Indeed, the biggest challenge in healthcare labor has persisted since before the pandemic: there are simply too few nurses and other clinicians for the rapidly growing workload. “Clinical shortages and nonclinical staffing shortages will persist through 2024,” reports accounting and advisory group LBMC.
The number of RN positions increased by 9.1% between 2012 and 2021, travel RN positions grew even faster (15.9%), and new positions are continuing to open at an accelerating rate.1 The U.S. Chamber of Commerce projects over 193,000 job openings for RNs per year through 2032.
But the staff just aren’t there. By 2032, the Chamber expects only a total of 177,400 nurses to enter the workforce, “less than what is needed to fill one year of projected openings.”1
These nurse shortages are hitting currently working nurses hard. For example, nearly all nurses report being regularly asked to cover extra shifts (85% say on a weekly basis).2 It also means that the workforce isn’t seeing any relief in their workload after having worked through the pandemic. The result: nurses are leaving.
%
77% say they are actively looking for a new job.
%
Nearly half (45%) say they plan to leave nursing altogether this year (2024).
%
That’s up from 34% who said the same thing in 2022.
All told, the nurse turnover rate ranges from 8.8% to as high as an incredible 37.0%1 More than half of all nurses leave their job within the first two years.1
That may also be why a million RNs with active licenses are not currently practicing.4 “It’s not because they don’t love nursing—they don’t love the stress, they don’t love putting their patients at risk, and they don’t love going home every day fearing that they had harmed someone,” NNU President Deborah Burger told Healthcare Dive.4
The main issue isn’t that nurses have given up on nursing; it’s that they want to see more sustainable staffing levels that allow them to focus on their work without risk of burnout. Consider: last year’s strike of New York nurses ended as soon as local health systems agreed to hire more nurses.5
Largely due to these labor issues, health systems will prioritize cost containment initiatives in 2024 and beyond.
Unfortunately, the consequences of nurse and clinician shortages aren’t just vacant roles and patient care being put at risk. They also include fast rising labor costs that, in the face of reimbursement changes reducing revenue, are putting the financial health of many healthcare facilities at risk.
Consequently, cost containment will necessarily remain a major driver of administrative healthcare decisions into the near future.
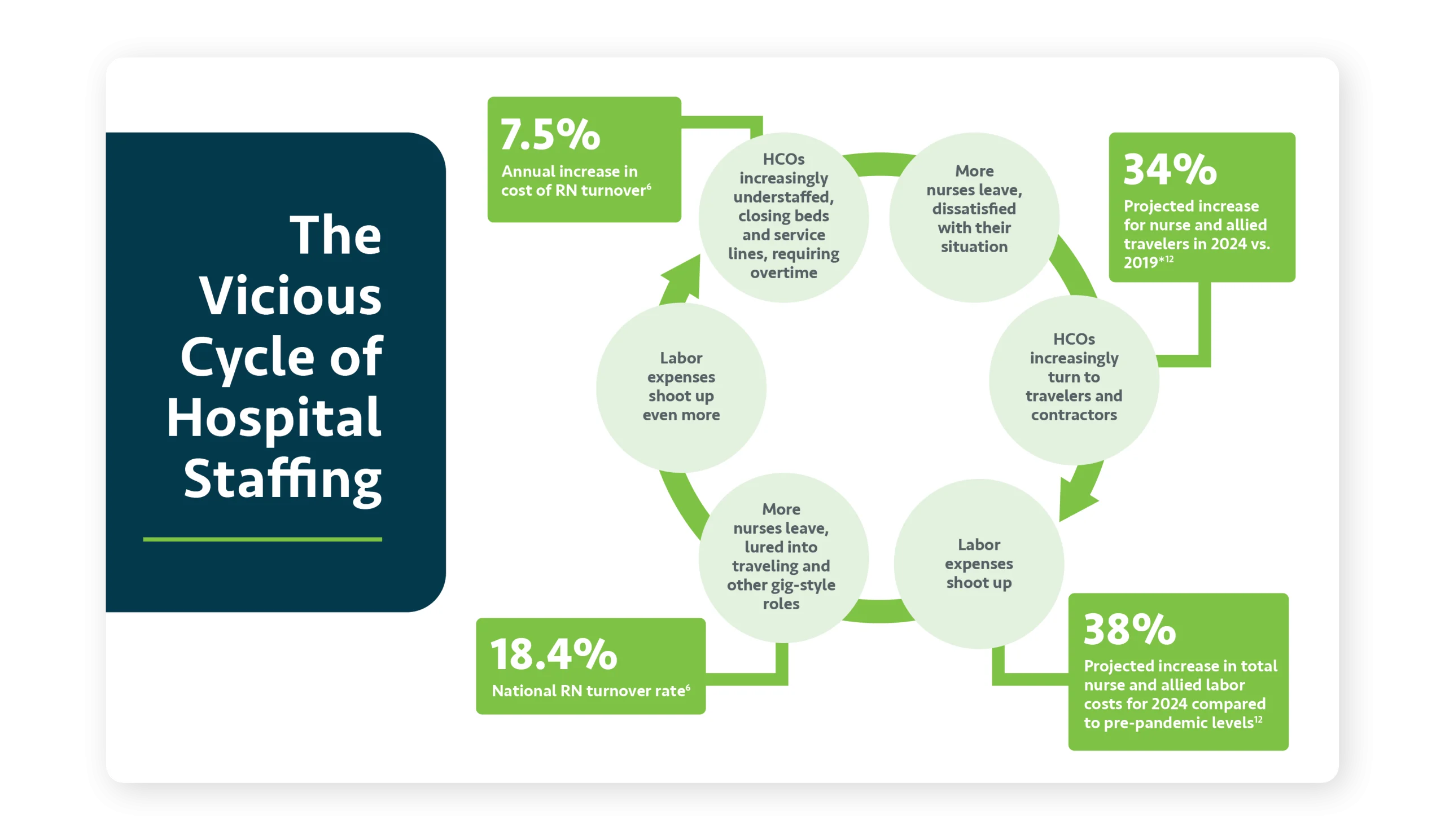
Right now, staffing in healthcare is acting out a sort of vicious cycle. More nurses leave (turnover), but fewer nurses are available, so vacancies increase. The current RN vacancy rate remains high at 18.4% nationally.6 As a result, hospitals and health systems have had no choice but to turn to costlier alternatives like contract, travel, and other similar nursing options. As those alternatives become more lucrative for the nurses, even more of them shift from full-time employment to those “gig”-style jobs, worsening turnover. The upshot: these are the kind of numbers that imperil operations and can force health systems to close beds, service lines, or entire locations.7
The situation wouldn’t be so serious if health systems had more leeway in generating revenue, but this too is an issue: “One of the significant regulatory factors impacting healthcare, particularly in rural areas, is the issue of Medicare cost reimbursement rates lagging behind the rising year over year cost to operate hospitals,” says Michael Yost, EVP, Chief Human Resources Officer at Great River Health, a health system serving a predominantly rural area including parts of Iowa, Illinois and Missouri.
Lessons Learned…or Ignored?
A year after the pandemic, labor rates have stabilized. And, while they remain higher than pre-pandemic, they have eased some. So it’s not all bad, right?
Amid the myriad of financial pressures healthcare organizations are facing, there is an inherent risk that they will view this rate stabilization as an opportunity to breathe a sigh of relief on contingent labor management issues and move onto other financial challenges. But that would be a grave mistake.
The pandemic showed that staffing agencies were all too willing to take advantage of the shift in supply and demand economics, recording record profits while health systems were at their most vulnerable. To combat this in the future, health systems must have the discipline to reduce their risk in this area, and future-proof their businesses. Reducing the over reliance on staffing agencies, and taking back control of contingent labor, is critical to managing overall costs.
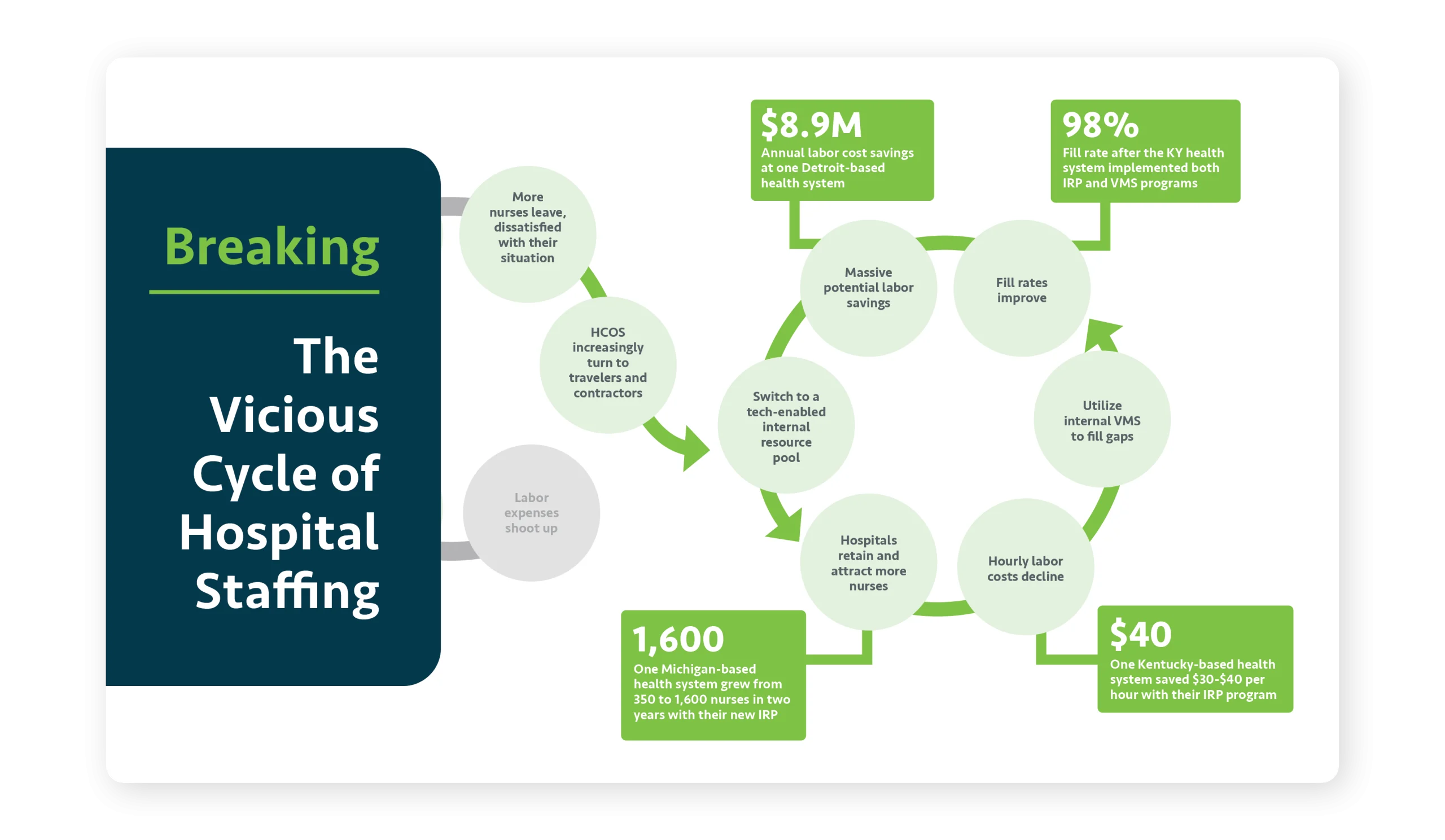
“Healthcare organizations must become much more attuned to reducing these costs while still meeting patient needs,” says Michelle Sanchez-Bickley, MS, SPHR, SHRM-SCP, Chief People Executive at Hallmark, “especially given that labor will remain one of the most significant expenses within healthcare for the foreseeable future.” Technology will necessarily play a role here. There’s just no way to interrupt the vicious cycle described above without (1) finding faster and more effective ways to recruit and (2) reducing administrative and clinical burden. Only purpose-built technology can do that and provide the leverage that is needed to break the cycle.
“Healthcare systems will continue to struggle with increased expenses and decreased reimbursement. Addressing this item will remain a top priority in 2024.”
– Michelle Hereford, MSHA, RN, FACHE System Chief Nurse Executive at University Hospitals Health System
“Healthcare systems will continue to struggle with increased expenses and decreased reimbursement. Addressing this item will remain a top priority in 2024.”
– Michelle Hereford, MSHA, RN, FACHE
System Chief Nurse Executive at University Hospitals Health System
The Solutions of The Future
Attracting nurses in this environment requires that organizations rethink staffing models to offer greater flexibility and other nurse-friendly characteristics.
The healthcare industry has permanently changed. Traditional staffing protocols are no longer sufficient to successfully attract nurses and other clinical talent. “We’re in an applicant market where demand greatly outweighs supply,” says Matt Dane, DNP, MBA, RN, Senior Vice President of Business Development at Hallmark. “Right now, we have to meet applicants where they are to attract them and provide what they want for their work-life balance.”7
Michelle Hereford, MSHA, RN, FACHE, System Chief Nurse Executive at Ohio-based University Hospitals Health System agrees. “We start by listening to the employee,” she says. “What is driving them? Money? Flexibility? Both? With that information, we help find the best assignment for that candidate.”
At Hereford’s organization, University Hospitals Health System, that has meant building an internal staffing pool of floating resources deployed throughout the organization. It’s the same at Great River Health. “Our organization has implemented several initiatives,” says Great River’s Yost, “such as offering competitive compensation packages and flexible working conditions to attract talent.”
At Franciscan Missionaries of Our Lady Health System in Louisiana and Mississippi, Annalee Starks, BSN, RN, System Director of Staffing, shares how she has created a single centralized staffing office to address their staffing challenges. “Creating a centralized staffing department for your entire organization, not just in each local market, enables insight into your greatest needs and oversight of where your contract labor spend is,” she says. “That kind of data will help you create strategies that will make large impacts to your facilities.”
In fact, building flexible employment models, internal resource pools, and even internally managed platforms for connecting with contract labor can beat the external agencies – that have been luring nurses away, and making clinical shortages worse – at their own game. This approach has the potential to move the needle. According to an analysis from McKinsey & Co., “meaningful work (82%) and flexible schedules (62%) are the most important factors that would influence surveyed RNs to stay in their position.”8
As a result, flexible staffing programs for nurses have the potential to break the vicious cycle described earlier. With more options to staff internally, healthcare organizations can reduce their reliance on travelers and agency nurses and access clinical staff at lower rates.
Just be aware that it’s not enough to just redesign staffing and workforce management models; new procedures and protocols must be operationalized, and that usually means utilizing purpose-built technology that can do more than scheduling software alone.
“I truly believe that leaders have to begin looking at how we hire differently. Thinking outside of the box and trying to meet those candidates where they are will offer a huge payoff in the end.”
– Annalee Starks, BSN, RN
System Director of Staffing at Franciscan Missionaries of Our Lady Health System
Success in future staffing rests on tech-enablement, including smart use of automation, AI, and other emerging technologies.
Technology is the foundation on which future solutions will rest. “Data analytics and AI can aid in resource allocation, patient management, and predictive healthcare,” says Yost. “Continuous investment in these technologies is vital for our future while balancing the rising cost of labor as a percent of our net revenue.”
For example, managing critical issues like credential and licensure expirations becomes increasingly difficult as health systems expand. Automated technology can track these issues and provide advance warnings when action is required by the organization. “If I had to do it manually, monitoring and tracking in real-time would be nearly impossible,” says Kim Sauro, former Director of the BestChoice System Float Pool at Michigan-based Henry Ford Health System.
Plus, automation will enable administrators to scale their own operations without necessarily having to add new FTEs to manage a growing workforce of contingent labor. Instead, equipped with the right tools, existing teams can make better use of existing administrative resources and be more effective in their roles. “The typical staffing practice is somebody sitting at a desk making phone calls, but we don’t have the luxury of that kind of time when we’re staffing five major hospitals and 200 ambulatory sites,” says Sauro. “Automating real-time communications via each clinician’s preferred channels (like email or text) is pivotal to reaching and attracting them.”9

![]()
“Developing streamlined ways to use both existing and emerging technologies can advance efficiencies for our staff and at the same time provide superb service to our patients and our customers.”
– Michelle Hereford, MSHA, RN, FACHE
System Chief Nurse Executive at University Hospitals Health System
One often under-appreciated approach to addressing modern clinical shortages: training, continuing education, and skills development.
Training and development programs can also help organizations build more resilient and adaptable workforces. Training programs can create ways to use existing resources more flexibly. For instance, a single nurse could be deployed in a wider range of situations or placed into different practice areas. Then, lower cost non-clinical staff can handle a wider range of tasks.
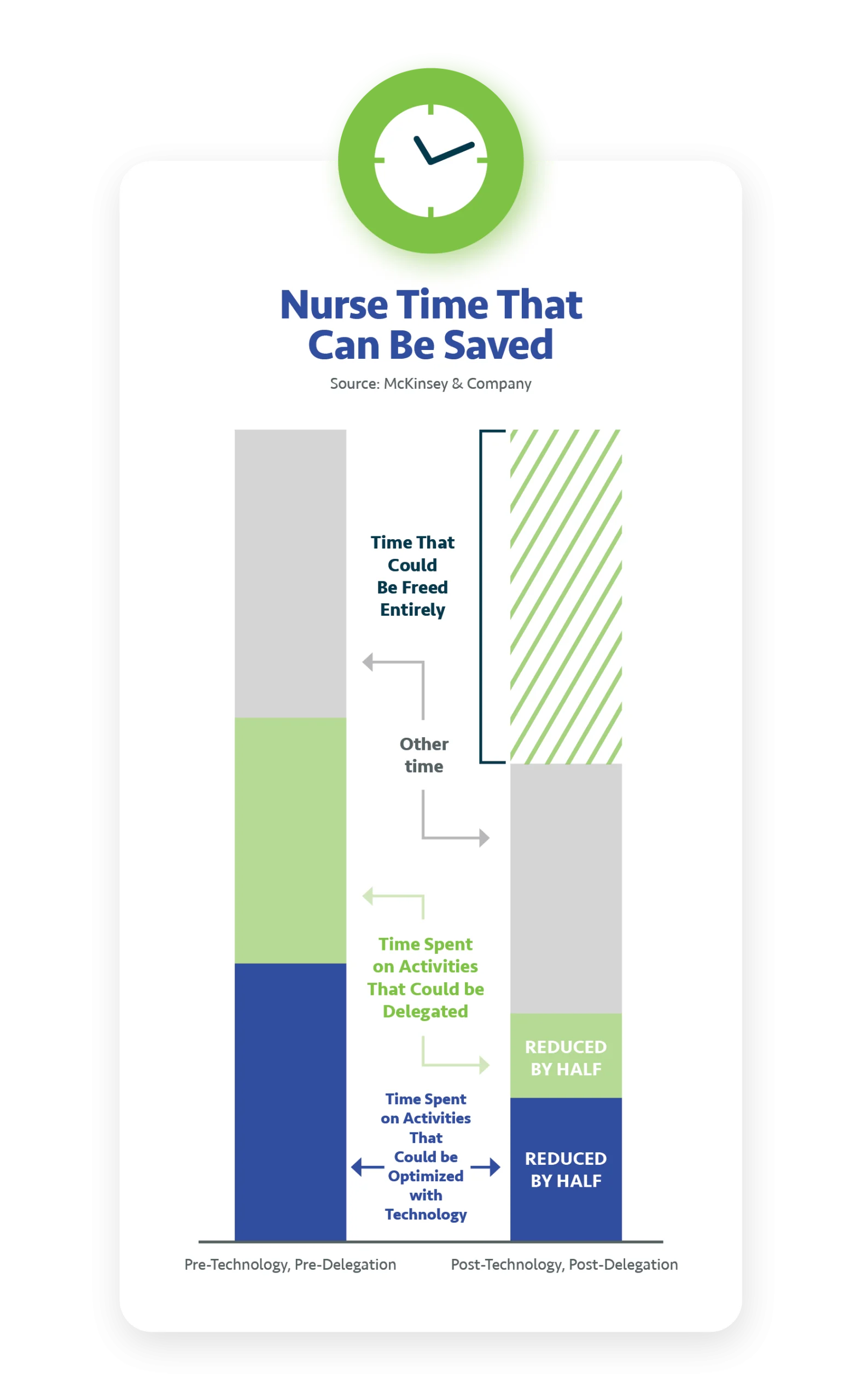
Expanding staff capabilities in this way can help “right- size” staffing by ensuring higher-paid clinical staff focus exclusively (or at least primarily) on higher-value activities and can be placed more flexibly as new needs arise. In turn, non-clinical tasks can be shifted to technicians and other staff. Analysts at McKinsey & Company suggest a combination of technology optimization and task delegation could save significant nurse labor (see chart).10
Additionally, training and skills development can help with retention and nurse satisfaction. One study of the retention effect of training found that training programs increased retention probability in the following calendar year by 8.8%.11 According to McKinsey, this is a priority for nurses, which would like to see the amount of time dedicated to their growth and development increase by 75%.10
The Path to Evolved Nurse Staffing
The path to a resilient, patient-centered, and financially sustainable healthcare system lies in the ability to adapt and innovate, while regaining control over contingent labor management. Flexibility and the willingness to embrace technological solutions like automation can help hospitals, health systems, and others successfully counter nurse shortages and related staffing challenges and tame the complexity of the modern healthcare landscape.
In particular, by building flexible employment models run through internal resource pools, organizations can replace or reduce the need to contract out to agencies in the first place and give nurses a more appealing work environment they actively want to join. For remaining needs, insourcing vendor management can then help organizations put open shifts up for bid to a variety of staffing agencies, using the power of free market economics to their benefit to drive down costs and reduce fill time. These solutions require a strategy to be paired with technology, but when successfully deployed, they can empower healthcare organizations to overcome clinical shortages – to enhance efficiencies, improve patient care, and navigate the difficulties of the modern healthcare landscape successfully.
Ultimately, only by addressing the pressing challenges of clinical shortages, cost containment, and operational complexities head-on can the healthcare sector chart a course towards a more sustainable, efficient, and patient-centered healthcare system where nurses are readily available, costs can be controlled, and quality care can be made accessible to the community.
To learn more about Hallmark’s workforce technology, contact us today or schedule a demo.
About the Contributors

Matt Dane
DNP, MBA, RN, Senior VP of Business Development - Hallmark
With in-depth expertise in sourcing and managing labor across all employment models, Matt leads market expansion for Hallmark by providing health systems and hospitals with a total contingent workforce management system for direct hire, freelance, gig economy worker, or agency contractor. Matt has nearly two decades of nursing experience, including serving as Chief Nursing Officer (CNO) for Baptist Inpatient Rehabilitation Hospital and Associate CNO for Baptist Memorial Health Care.

Michelle Hereford
MSHA, RN, FACHE, System Chief Nurse Executive - University Hospitals Health System
Michelle joined UH in April 2021 as Chief Nursing Executive, responsible for overseeing nursing operations, professional practice, education, and research. With nearly three decades of experience in diverse healthcare settings, including academic medical centers and community hospitals, she brings expertise in enhancing patient-centered care and clinical quality. She holds a BSN and MSHA from Virginia Commonwealth University/Medical College of Virginia and is a fellow in the American College of Healthcare Executives.

Michelle Sanchez-Bickley
MS, SPHR, SHRM-SCP, Chief People Executive - Hallmark
Michelle is an HR executive with nearly 30 years’ experience in Human Resources. She has a strong background in strategic planning and developing and implementing innovative solutions to achieve business objectives. At Hallmark, she works with healthcare executives nationally to provide a total contingent workforce management system that streamlines processes and reduces costs. Prior to her current role, Michelle was a CHRO for a health system, overseeing all aspects of Human Resources within the integrated health system.

Annalee Starks,
BSN, RN, System Director of Staffing- Franciscan Missionaries of Our Lady Health System
Annalee Starks, BSN, RN, has amassed over 20 years of healthcare experience, ascending from an ED unit secretary to positions such as Dialysis and Hospital Administrator. Her illustrious career includes managing hospital departments for over a decade, receiving prestigious accolades like the Great 100 Nurses of Louisiana, Nurse Leader of the Year Nightingale Award, and earning the title of Baton Rouge Nurse Manager. Currently, as the Director of the staffing program at Franciscan Missionaries of Our Lady Health System, Annalee combines her extensive healthcare management background with a deep understanding of staffing agency dynamics, embodying leadership, excellence, and a sincere dedication to impacting the healthcare community positively.

Michael Yost
EVP, Chief Human Resources Officer - Great River Health
Michael Yost is an accomplished executive with over 18 years of experience in human resources. Currently serving as the Executive Vice President and Chief Human Resource Officer for Great River Health System, Michael brings extensive experience and a proven track record of success to his role. Before his tenure at Great River Health System, Michael held senior HR leadership positions at three prominent health systems across the country, where he played a pivotal role in shaping organizational culture, talent initiatives, and strategic workforce planning.
References
- Hoover, Makinizi; Mahoney, Katie; & Lucy, Isabella. “Data Deep Dive: A National Nursing Crisis.” U.S. Chamber of Commerce. 29 Jan. 2014, https://www.uschamber.com/workforce/nursing-workforce-data-center-a-national-nursing-crisis
- Roques, Danielle & Zheng, Katherine. “Nursing Trends: 2024 Report for Healthcare Employers.” IntelyCare. 2024,
https://www.intelycare.com/facilities/resources/nursing-trends-report-for-healthcare-employers/ - Landi, Heather. “Third of nurses plan to leave their jobs in 2022, survey finds.” Fierce Healthcare. 22 Mar. 2022,
https://www.fiercehealthcare.com/providers/third-nurses-plan-leave-their-jobs-2022-survey-finds - Mensik, Hailey. “Lawmakers to reintroduce federal nurse staffing ratio bill.” Healthcare Dive. 30 Mar. 2023,
https://www.healthcaredive.com/news/federal-nurse-staffing-ratios-bill-reintroduced/646426/ - Otterman, Sharon; Goldstein, Joseph; & Gross, Jenny. “Nurses’ Strike Ends in New York City After Hospitals Agree to Add Nurses.” The New York Times. 12 Jan. 2023, https://www.nytimes.com/2023/01/12/nyregion/nurses-strike-ends-nyc.html
- NSI Nursing Solutions, Inc. “2024 NSI National Health Care Retention & RN Staffing Report.” 2024,
https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf - Hallmark. “How to Minimize Impact of Nurse Shortages on Your Hospital’s Service Lines.” 22 Mar. 2023,
https://blog.hallmarkhcs.com/how-to-minimize-impact-of-nurse-shortages-on-your-hospitals-service-lines - Hallmark. “Counter Labor Shortages and Improve Staff Retention in Health Care.” 27 Sep. 2023,
https://blog.hallmarkhcs.com/counter-labor-shortages-and-improve-staff-retention-in-health-care - Hallmark. “3 Key Takeaways from ‘The Power of Tech-Enablement: Modernizing Today’s Mobile Workforce.” 25 Oct. https://blog.hallmarkhcs.com/3-key-takeaways-from-the-power-of-tech-enablement-modernizing-todays-mobile-workforce
- Berlin, Gretchen; Bilazarian, Ani; Chang, Joyce; & Hammer, Stephanie. “Reimagining the nursing workload: Finding time to close the workforce gap.” McKinsey & Company. 26 May 2023, https://www.mckinsey.com/industries/healthcare/our-insights/reimagining-the-nursing-workload-finding-time-to-close-the-workforce-gap
- Dietz, Daniel & Zwick, Thomas. “The retention effect of training: Portability, visibility, and credibility.” The International Journal of Human Resource Management Volume 33, 2022 – Issue 4. 10 Apr. 2020, https://www.tandfonline.com/doi/full/10.1080/09585192.2020.1737835
- William Blair. “Proprietary Nurse and Allied Staffing Industry Penetration Model: Is the Industry Approaching a Bottom?” 1 Apr. 2024.