Experts weigh in on the future of nursing contingent labor and workforce strategy in new report
The healthcare industry may be facing an inflection point in nursing contingent labor. Nurses and other clinicians remain scarce, with high turnover rates and increasing staff shortages persisting. And while contingent labor rates have softened some over recent months, they remain higher than they were pre-pandemic. These factors, coupled with changes in reimbursement that threaten income, are jeopardizing the financial viability of many hospitals and health systems. The good news is that there are ways out of this vicious cycle. For example, developing flexible work arrangements for nurses seeking greater autonomy and deploying innovative technologies can enable healthcare organizations to achieve and improve both financial stability and clinical excellence.
To help hospitals and health systems navigate the modern landscape of nursing contingent labor, Hallmark surveyed a panel of healthcare industry experts. We have collected their input into the 2024 edition of our annual Outlook on Contingent Labor in Healthcare report. This publication delivers an in-depth, expert-driven analysis of the challenges, trends, and opportunities for hospitals and health systems—and offers a roadmap for solutions to existing and emerging nurse labor challenges.
Here are three key takeaways from the 2024 Outlook Report on Healthcare Contingent Labor:
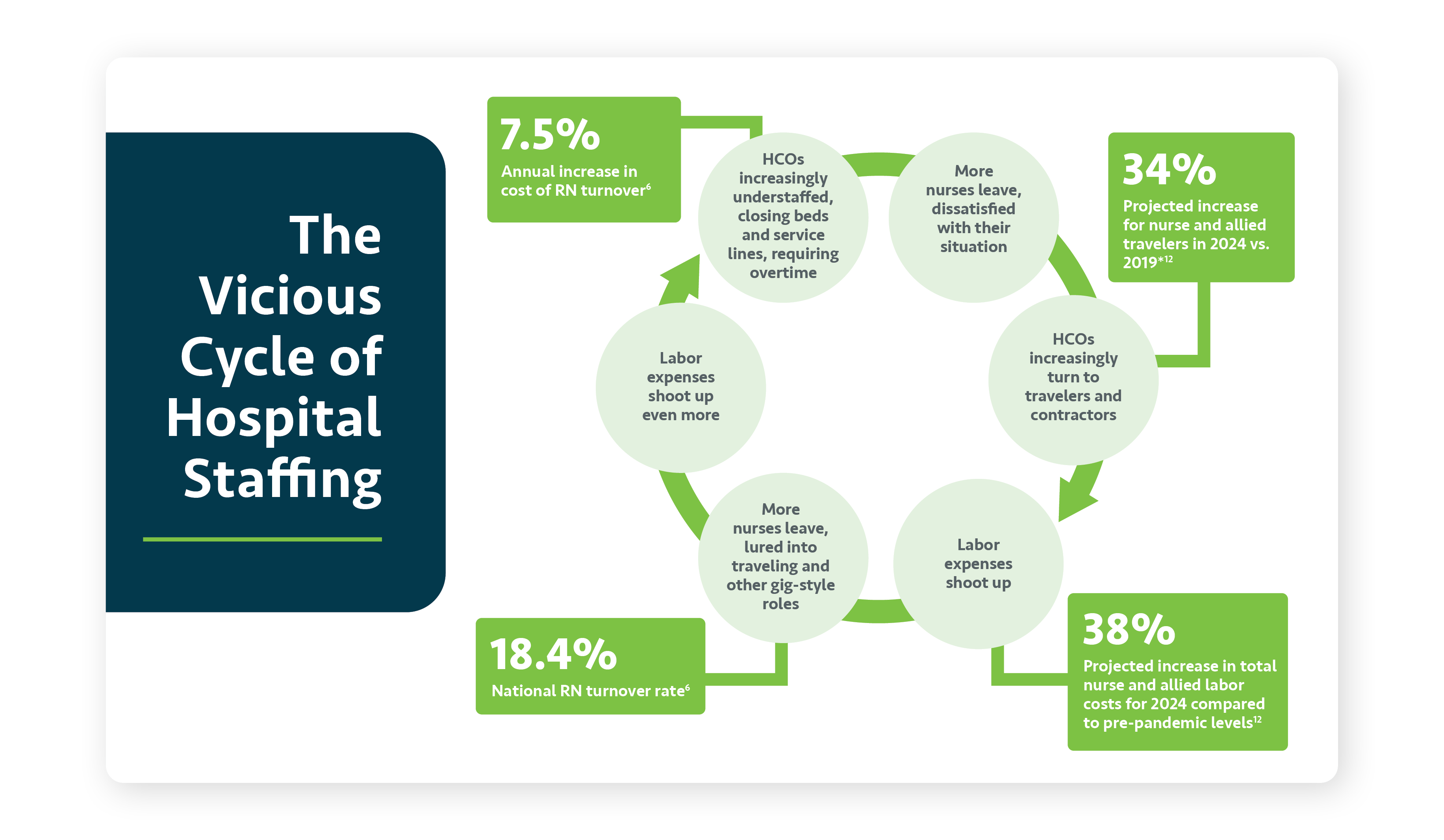
1: Much of the industry is caught in a vicious cycle of rising expenses for nursing contingent labor and worsening turnover
When it comes to nursing staff, shortages beget shortages. As dissatisfied nurses leave, systems have no choice but to turn to agency nurses and travelers. A 138.5% increase in nursing contingent labor compared to before the pandemic—causing labor-related expenses to remain high. In turn, even more nurses leave the profession, either burned out entirely or lured into more flexible and higher-paying gig-style roles. As a result, labor expenses shoot up even more.
In extreme cases, this can leave hospitals forced to close beds and service lines. In addition, they may require more overtime from their existing nursing staff (85% of nurses say they are asked to cover extra shifts every week), which burns out and disengages even more nurses. It is a tough nurse workforce management cycle in which many systems are currently trapped.
2: Consequently, the top labor priority for nurse contingent labor is breaking this cycle
If nurses are leaving due to overwork or because they have been enticed by the flexibility and high pay of contract roles, how do hospitals and health systems break the cycle described above? “We start by listening to the employee,” Michelle Hereford, MSHA, RN, FACHE, System Chief Nurse Executive at Ohio-based University Hospitals Health System, told us. “What is driving them? Money? Flexibility? Both? With that information, we help find the best assignment for that candidate.”
This process will necessarily include designing employment programs that offer what those nurses want, so they can work as much or as little as they choose. “Leaders have to begin looking at how we hire differently,” says Annalee Starks, BSN, RN, System Director of Staffing at Flex Choice Staffing for Franciscan Missionaries of Our Lady Health System. “Thinking outside the box and trying to meet those candidates where they are will offer a huge payoff in the end.”
3: Tech-enabled contingent labor management is more important than ever
Technology is the foundation on which future solutions will rest. It would be impossible to break this vicious cycle and keep up with labor needs—much less outcompete others—without the smart use of enabling technology. “Developing streamlined ways to use both existing and emerging technologies can advance efficiencies for our staff and at the same time provide better service to our patients and our customers,” says Michelle Sanchez-Bickley, MS, SPHR, SHRM-SCP, Chief People Executive at Hallmark.
There is no single technology solution or platform that will solve all problems for all health systems. However, all health systems will need some form of technology to operationalize their newly designed nurse workforce management programs. The good news is that there are very sophisticated platforms available that can allow health systems to retain more staff and compete directly with managed service providers and agencies.
These takeaways are only the start.
The full Hallmark 2024 Outlook for Nursing Contingent Labor Report also addresses questions like:
- What is the state of nurse shortages, turnover, and retention?
- What role will training programs and skills development play in improving the labor situation?
- How can organizations operationalize new flex programs for contingent labor?
- How is merger and acquisition activity affecting the labor landscape?
Explore these topics and more by downloading the full report.